Get In-depth Biotech Coverage with Timmerman Report.
24
Apr
2023
Gene Editing Therapies Delivered In Vivo: Ensoma’s Emile Nuwaysir on The Long Run
Today’s guest on The Long Run is Emile Nuwaysir.
Emile is the CEO of Boston-based Ensoma.

Emile Nuwaysir, CEO, Ensoma
Ensoma is developing gene-editing therapies that can be delivered in a single shot, in vivo, inside the body. The name is derived from the Greek word for ‘in the body.’
The basic idea is to make these gene editing medicines so they can be given off-the-shelf, to any patient, and that they can deliver a fairly long and complex set of genetic instructions in a single shot.
The hope is to deliver these treatments — which you could call a genetic form of surgery — without having to go through the steps common to some of the first-generation gene editing procedures, which are often performed outside the body, or ex vivo.
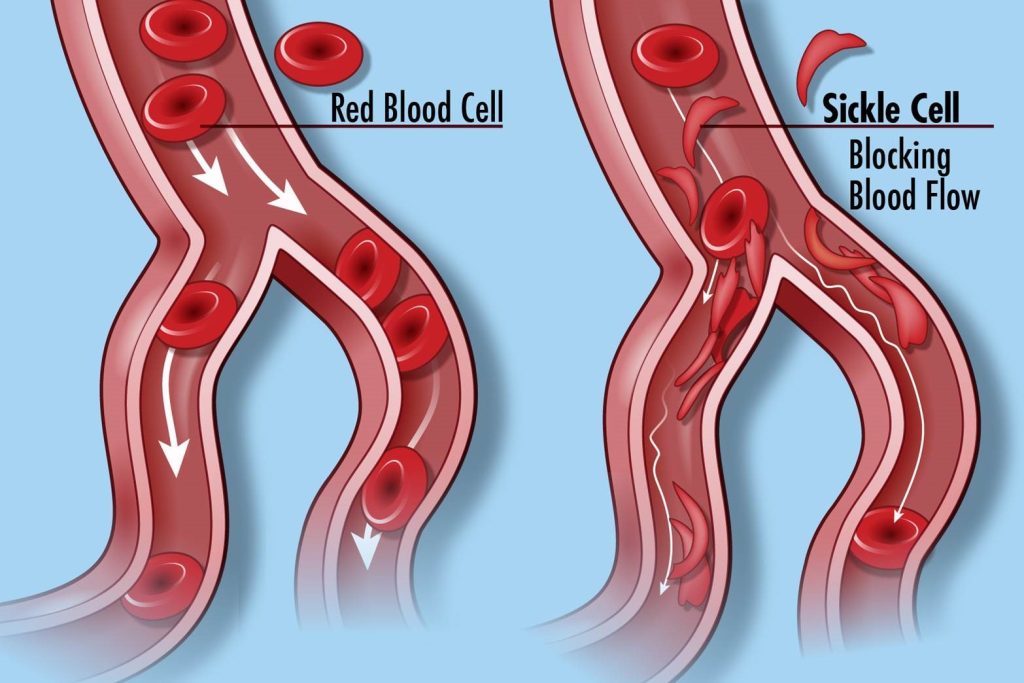
Some of the well-known variations on CRISPR gene editing require a patient to undergo a blood draw, have certain cells isolated — like hematoepoeitic or blood-forming stem cells, for example. Then the patient undergoes another procedure, such as chemotherapy preconditioning, before the engineered cells can be re-infused back.
That takes time and money. It’s a process that has to be carefully choreographed. It’s not likely to ever reach global scale, like in poor countries that might someday want access to the curative power of gene editing therapies. Ensoma hopes to eliminate the need for those blood withdrawals, and preconditioning therapies, and re-infusions. It wants to deliver the gene editing therapy once, and in a single shot.
Emile is a scientist by training, with a PhD in molecular toxicology with a focus on oncology from the University of Wisconsin-Madison. He has been through a series of startups that have given him a wide variety of experiences in genomics, diagnostics, cell therapy, and antibodies. He’s been a part of three startups that were ultimately acquired by big players – Roche, Fujifilm, and Bayer. From 2021-2022 he was chairman of the board for the Alliance for Regenerative Medicine.
None of this was preordained or predictable when he first got interested in science. Like so many scientific entrepreneurs, he discovered his technology interests and inclination to work in startups along the way.
And now for a word from the sponsor of The Long Run
Occam Global is an international professional services firm focusing on executive recruitment, organizational development and board construction. The firm’s clientele emphasize intensely purposeful and broadly accomplished entrepreneurs and visionary investors in the Life Sciences. Occam Global augments such extraordinary and committed individuals in building high performing executive teams and assembling appropriate governance structures. Occam serves such opportune sectors as gene/cell therapy, neuroscience, gene editing, the intersection of AI and Machine Learning and drug discovery and development.
Connect with them at:
www.occam-global.com/longrun

And do you want to be a part of the world’s largest biotechnology industry event?
Come to Boston from June 5 to June 8 for the 2023 BIO International Convention. Join over 14,000 biotech leaders from dozens of countries, for one week of partnering, networking, and robust educational sessions.
With unparalleled networking events like the receptions at Boston’s premier music hall “Big Night Live” or the party at the “MGM Fenway Music Hall”, This is the place you’ll want to be this June.
Register today at:
bio.org/events
Now, please join me and Emile Nuwaysir on The Long Run.