Controlling COVID in 2022: Masks, Treatments and Fast, Frequent Testing

Mara Aspinall, managing director, BlueStone Venture Partners; professor of the practice, biomedical diagnostics, Arizona State University
Over the past week I have been reflecting on what we know now, two years into a seemingly unending pandemic.
One of the biggest failures has been with testing.
At first, our only effective defenses were masking and social distancing. We were slow to ramp up testing, unable to give most people the timely information they could use to isolate and curb the spread.
As the first year went on, we got better and better at testing. First came PCR, then rapid antigen tests.
At the start of 2021, we began to think that testing was less necessary. Vaccination, many hoped, would bring the end of COVID all on its own. Masking became inconsistent and despised. Testing declined – to the extent that a major US rapid test antigen company began to wind down a manufacturing plant in the summer of 2021.
Now at the end of 2021, it is clear that the virus has continued to evolve in dangerous ways.
It has kept pace, and in some ways is outpacing our best efforts. Rapid antigen tests are now reportedly in short supply in many parts of the country, right at the time they are needed most. New more transmissible variants are emerging every ~100 days. The newly emergent Omicron variant contains all the best/worst mutations of earlier variants that contribute to transmissibility and immune escape, plus an unprecedented number of mutations of which we know little or nothing.
Today, the CDC reported that Omicron makes up about 73 percent of new US cases. It took two weeks to reach that threshold. Delta needed four weeks to reach that level, and Alpha took 12 weeks. [Clarification, 12:40 pm PT Dec. 28: On Dec. 28, the CDC revised this estimate of Omicron incidence downward from 73 percent to 23 percent of new cases for the week ending Dec. 18.–LT]
In 2022, we will add effective treatments for the more seriously ill. But instead of putting all our eggs in one basket, we must mobilize all the tools at our disposal to return to “normal”, whatever that will turn out to be. Masking, vaccination, improved indoor ventilation, and the fast, low-cost and frequent self-testing that empowers individuals to manage their own health, their family health, and their community health.
Effective testing depends on how, when and where the virus replicates and the natural progression of resulting infections. A major challenge to our early understanding was that all our data came only from the sickest patients in hospital.
How did testing become so much easier, simpler and cheaper?
We have decent answers to four key scientific questions that put us in much better position than we were in two years ago:
- How is the virus transmitted? Primarily aerosols, less so bodily fluids, and rarely fomites.
- From where can we acquire a valid sample? Upper respiratory tract tissue secretions: mucus and saliva. There’s no need for more invasive or difficult to obtain biopsies or bronchoscopy.
- Which infection products are reliable analytes? mRNA and N proteins, much less so immune response markers such as IgM from blood or volatile metabolic by-products from breath.
- Are there easy to observe symptoms that are sufficiently reliable to act as a proxy for the infection itself? Unfortunately, no, not this time around, the only unique symptom is loss of smell or taste, but this is not universal. Temperature monitoring that worked well for SARS-CoV-1 in 2003 is largely futile “hygiene theater” for COVID-19. It’s not sensitive and not specific enough to be useful even as a screening test.
Stopping the chain of transmission requires tests that identify the infectious subset of the infected. If the upper respiratory viral load is high enough, secondary aerosol transmission can occur, especially in closed spaces where vocalization is happening (e.g. choirs, basketball arenas, bars and restaurants).
High viral loads have been identified in all infectees: vaccinated or not; asymptomatic, pre-symptomatic, peak symptomatic, or early post symptomatic. This is to be expected, as the vaccines were designed to stimulate systemic immunity to save lives – they weren’t designed to prevent infection and transmission (although some scientists hoped they might do it all).
Optimizing the testing protocols for increasingly available rapid antigen tests depend on studies of the end-to-end natural history of disease in the same individuals over time (i.e. longitudinal, not cross-sectional) — from pre-infection, first positive test, peak infection, through viral clearance across all degrees of illness severity. This data is harder to find, mainly because it’s harder to collect than cross-sectional data.
But we do have some data to help guide us here.
A July 2021 Singapore study of hospitalized patients with Delta variant infections, who were previously given mRNA vaccines, showed that peak viral loads were similar between vaccinated and unvaccinated patients, but that the vaccinated had less severe illness and cleared the virus consistently faster (see adapted study Fig. 1).
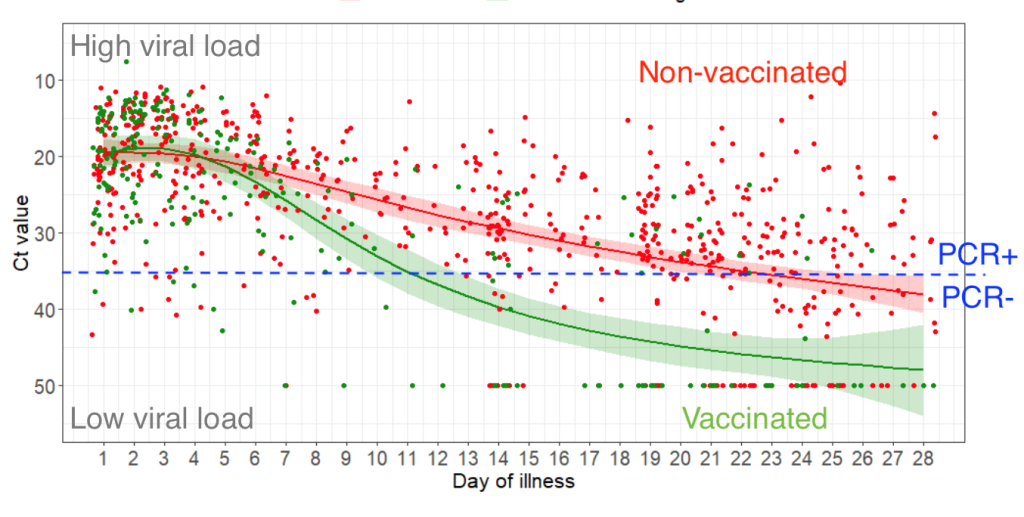
Fig. 1. Virological and serological kinetics of SARS-CoV-2 Delta variant vaccine-breakthrough infections: a multi-center cohort study. MedRxiv. July 31, 2021. (Barnaby Edward Young et al National Center for Infectious Diseases, Singapore).
One caveat: only the seriously symptomatic were included in this study.
A December 2021 letter in the New England Journal of Medicine confirms these insights in the National Basketball Association’s 2020/2021 longitudinal screening program in a group of 173 healthy individuals (60% players/40% staff), PCR tested 19,941 times (before Omicron emerged):
- On average, from first contact through viral clearance takes an average of 13 days for the vaccinated and 15 days for the non-vaccinated – 4 days from contact to 1st PCR+; 3.2-3.5 days to peak viral load; 5.5-7.5 more days for the unvaccinated to clear the virus. These estimates combine the results of a comprehensive study of a May/June 2021 Delta outbreak in Guangdong, China (30 million unvaccinated community PCR tests and 100% contact tracing of all 167 cases) that found that infectious contact to 1st PCR+ in the 25% who developed COVID took an average 4 pre-symptomatic days. These data from China are consistent with the NBA study results of 1st to last PCR dynamics, published in the NEJM. The NBA study found that 1st PCR+ to peak timing was similar for both vaccinated and unvaccinated but that the vaccinated cleared the virus 2.3 days faster, with less patient-to-patient variation (see adapted Fig 1D & E). Several unvaccinated patients (Figure S7) had particularly long clearance times with PCR-detectable virus up to 30 days post-peak.
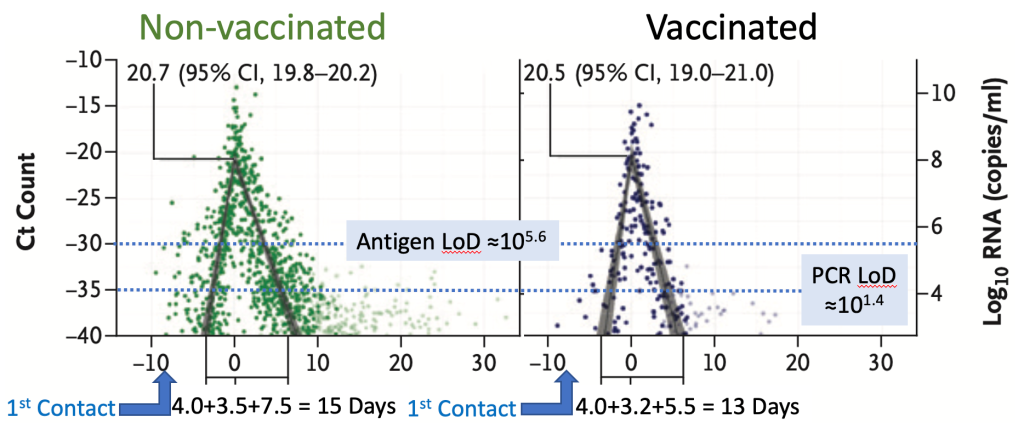
Adapted Fig. 1 and 2. Viral Dynamics of SARS-CoV-2 Variants in Vaccinated and Unvaccinated Persons. NEJM. Dec. 1, 2021.
- Peak viral load tops out around 100 million to 1 billion viral copies per ml (108 – 109cp/ml) and “…found no meaningful difference…” across all sub-groups sampled: vaccinated or not, and across variants (Wuhan A/B, Alpha or Delta – Figure 1F). However, through the wonder of exponential scales, it is worth noting that the 108.0 cp/ml in the vaccinated is still 20% less virus than the 108.1 cp/ml in the unvaccinated. In contrast to the NBA study, two earlier studies found greater differences in viral load: year-end 2020 Alpha surge data from Israel (May 2021 Nature Medicine) estimated 2.8-4.5x lower viral load in vaccinated patients (perhaps because mRNA vaccination was more effective at clearing Alpha variant infection?); and the Guangdong, China study found Delta peak viral load to be ~1,000x (103) that of the initial Wuhan A/B D614G strain (24 cycle threshold (Ct) versus 34Ct). Either way, there is no doubt today that we have to assume that all infected individuals can reach similar viral loads and be infectious whether vaccinated or not, and whether asymptomatic or not. In other words – test, test, test to detect infection early so people can isolate in a timely manner.
- Rapid antigen tests are sensitive enough to detect transmissible individuals. A May 2021 study published in The Lancet showed there is a consensus that viral load drives transmission: the secondary attack rate (% contacts infected) was 24% if the index case viral load was >1010 cp/ml but only 12% if <106 cp/ml. The Roche Cobas PCR test used in the NBA data has a limit of detection of ~25 cp/ml (101.4 cp/ml), corresponding to ~35 cycle threshold (Ct) (see the study’s methodology in supplementary data). Rapid antigen tests are typically 10,000x less sensitive, i.e. are antigen positive >105.4 cp/ml. Laboratory culture of virus is typically unsuccessful <106 which implies a negative antigen test represents inability to transmit between humans, at the time of the test. This is evidence that the rapid tests are giving us valuable information – they tell us whether we are infectious at a given moment.
- Frequent testing is essential because viral load increases fast. In the NBA group, each new variant has shortened the time from 1st PCR+ to peak viral load. The ramp-up is remarkably fast. The Wuhan D614G variant took an average of 4.2 days from 1st PCR positive to peak viral load; Alpha 3.4 days; and Delta 3.0 days. It is likely that Omicron will prove faster still – if so, the good news is a shorter pre-symptomatic but transmissible delay, but the bad news is that it enables faster surge growth. Billy Quilty, a researcher at the London School of Hygiene & Tropical Medicine demonstrated this by taking a rapid antigen test 4 times in 24 hours, which was likely Delta, but might have been Omicron (no sequencing or PCR SGTF was performed to confirm the presence of Omicron).

Based on these data, we can conclude a few things.
Vaccines are still extremely valuable tools, but they are one layer of protection out of many.
To curb the rate of spread and keep our hospitals from being overwhelmed, we need to massively increase both the number of people who test, and how often we test, while being highly diligent in masking – even for the vaccinated and boosted. Otherwise, we’ll continue to fly blind during another very long and painful winter.




