Team Julie: Fighting Back Against Glioblastoma

Scott Rakestraw
Thirty-seven years ago, I met a lovely and talented young woman while we were both pursuing our PhDs.
We were married during our last year in graduate school, and have spent every day since raising a family; working in STEM-Medicine careers; and engaging with our communities.
We had just retired in 2019 and begun making plans to travel and enjoy life when COVID hit.
Then came the “Big One.”
Last December, my wife Julie was diagnosed with glioblastoma multiforme (GBM), the same aggressive brain cancer that killed President Biden’s son Beau, and Senators Ted Kennedy and John McCain.
Our lives changed forever. Where do we go from here?
The instant the MRI came back, it was clear that Julie had glioblastoma. That image delivered a gut punch. My experience as a biotech executive, investor and advisor has taught me that standard treatments of the past 30 years offer only marginal effectiveness, and most experimental agents fail. Julie’s case looked particularly grim at first glance: the tumor was large enough (5 centimeters in diameter) that it was pushing a significant portion of Julie’s left cerebral hemisphere into the emergent Danger Zone of fatal brain herniation.
We would have to act fast. But first, I had to make a phone call no father ever wants to make.
I stepped out of the ER to call our children, Dr. Stephanie Rakestraw, a general surgeon in Alabama, and Alex Rakestraw, an advertising strategist and writer in New York. Videos of Julie’s MRI scans popped into our “Dad and Kids” group text as I told them what those scans showed. You could hear a pin drop. They weren’t going to wait for Christmas to see their Mom. The kids quickly booked predawn flights – they would be home in Bucks County, Pennsylvania, no matter what.
Well after midnight, I drove home from Princeton, NJ. I pulled some leftovers out of the fridge, poured a stiff drink, and lay down alone in bed for a few minutes. Sleep was impossible. I had to clear my head enough to start critically thinking about the road ahead as a caregiver, husband, father and patient advocate.
The amazing Joanne Smith-Farrell, CEO of Be Biopharma and a friend, calls this process “The Journey,” a road traveled by all spouses/partners of a critically ill cancer patient. Early the next morning, The Journey began.
The kids drove straight from the Philadelphia airport to the Thomas Jefferson University Neuro ICU. I met them in the lobby and filled them in with all the composure I could muster: Mom had been transferred overnight from the local hospital ER, and was being evaluated for emergency neurosurgery. Given the tumor size and location, we would be fortunate to have Julie recover from the surgery without severely compromised speech/language and executive function capabilities. A world-class neurosurgeon might be able to perform a maximal safe resection that would remove perhaps 90% of the tumor. David W. Andrews, MD is one of the best: the surgery was a success.
That bought us some time. But there wasn’t time to waste. We had to think about what to do about the cancer cells that remained, and how to best neutralize the threat they posed.
It is useful to keep in mind that cancer is a deeply personal disease – that is, in fact, part of its wickedness. Each cancer displays its own cellular and molecular profile. That means that even while we rely on well-controlled clinical trials to guide best treatment practices, those studies only provide us with rough guidelines based on the best odds in fairly heterogeneous patient populations. The true therapeutic protocol for every individual cancer patient is essentially an “N-of-1” uncontrolled clinical experiment, usually involving multi-agent combination therapy. There are always adverse events to consider, especially with cancer treatment. They need to be managed carefully, because quality of life matters. No one wants to live a few extra months if those extra months are utterly miserable.
To find the right path for Julie, we leaned on all of our knowledge and contacts from the past 30 years in biotech. First, we had to send a tissue sample taken during Julie’s neurosurgery to multiple labs for extensive molecular and genetic profiling.
While we waited for results, the family made the best of a holiday no one had planned: both kids, their significant others, and Tony the Cat unwrapped presents Christmas morning. Even though our lives had changed, life itself was worth celebrating. We savored every minute.
The results came back right after the New Year. I had some idea of where to begin, but quickly needed the counsel of experts to efficiently “Boil the Ocean” to map out Julie’s treatment plan. Dozens of emails and text messages were sent out worldwide asking for quick turnaround Zoom sessions and telephone calls. Team Julie began to respond immediately, often within minutes. Senior life sciences leaders across both industry and academia, usually asked a simple question: “How can I help?” And, without requests from me, they took their own initiative, inviting their colleagues to help chart the best course for Julie.
Behold: The true power of knowledge and empathy within our industry.
Upon seeing the molecular and genetic profiling of Julie’s tumor, #TeamJulie quickly crafted a plan to venture “off the map.”
Simply put, sticking with the post-radiation adjuvant portion of the standard of care Stupp protocol alone was not going to be a winning strategy given the molecular and genetic data. A multi-component treatment plan was crafted based on the tumor profile data.
One key component is the Optune device, a cap that sends alternating electrical pulses through the brain to slow or stop the out-of-control cell division of the tumor. Because Julie’s tumors appeared to express high levels of PD-L1, she was a good candidate for treatment with the PD-1 inhibitor pembrolizumab (marketed by Merck as Keytruda). She also got fluoxetine, a generic selective serotonin reuptake inhibitor that’s commonly taken by brain cancer patients to stabilize mood (and has recently been shown to inhibit EGFR signaling in GBM cells), and also infliximab, the Tumor Necrosis Factor inhibitor marketed by Johnson & Johnson as Remicade. (For more about the specifics of the treatment plan, visit MissionGBM.)
This treatment plan has not been without its setbacks – after all, there is nothing more complex than human biology, especially when that biology is being turned against itself by cancer.
Julie has a hyper-sensitive innate immune system. While checkpoint inhibitor immunotherapy is generally well tolerated, we managed to blow up Julie’s thyroid and sigmoid colon with Grade 3+ immune-related serious adverse events on Cycle 1 of immunotherapy. But she recovered and we kept our eyes on the horizon. The silver lining: extensive published clinical research regarding immunotherapy of cancer patients shows that the patients displaying the most aggressive immune-related adverse events are also the ones who tend to have the best objective tumor responses.
Some breathtaking science led us to create this personalized treatment plan. The tools of diagnosis and treatment are far more advanced than they were a decade ago. Even so, as good as it all sounds on paper, it took a lot of Julie’s courage to continue trusting the same knucklehead (#Husband) who hospitalized her early in her treatment.
Our Journey is now approaching the one-year mark. Julie is clinically stable, active, feels good, walks 3-4 miles per day with occasional Peloton cycling sessions. She is enjoying each day despite the constant presence of her tumor (now lovingly nicknamed “Glio”). In September, Stephanie and Alex made an emotional trip home to celebrate their Mom’s 59th birthday with cake, laughter, and joy.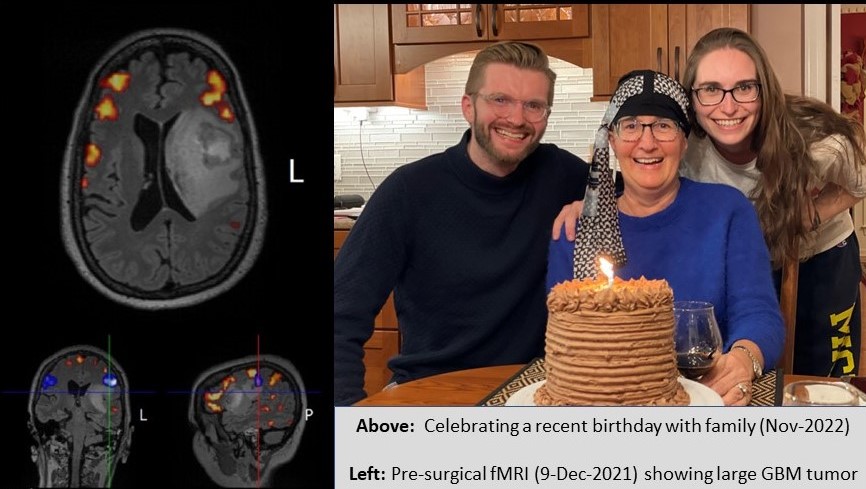
The big smiles underscore commemoration of a birthday that few people believed Julie would see. Those smiles are a direct result of some incredible and selfless work performed by countless many in our industry. You know who you are, and what you have done. We invite the reader to read “An Open Letter to Team Julie” to learn more about the people and leading-edge science behind Julie’s customized therapeutic protocol. You are all #BeyondGreat. We are forever in your debt.
That said, we are not naïve: GBM has a one-year survival rate around 20 percent with a five-year survival rate in the single digits. The Journey will undoubtedly be tortuous. However, how we live between now and then is not up to a disease. It is up to us. And we get by with a little help from our amazing friends and colleagues in the biopharma and biomedical industries.
Julie and I have increased our focus on spending time with family and friends, and making every day count. In addition, I have come out of retirement and am riding herd to inject significant new scientific and capital resources into brain cancer therapeutics innovation.
Julie’s cancer makes it clear that none of us are guaranteed tomorrow. Be sure to live your life, enjoy each day, and pay it forward if you are able. Julie has embraced her love of photography. Her daily walks are now spent with camera in hand, capturing the turtles, wildflowers, and Great Blue Herons that surround our home.
One day, there may be no more cards to play – and yet, we will be at the final table. You will know it is us: I will be the player betting all his chips on each hand, and Julie will be right there with me. None of this would be possible without the dedicated people who answer the call every day in our chosen industry.
To follow Scott and Julie’s Journey, visit MissionGBM. At MissionGBM, the objectives are (1) to raise awareness of advances in the development of brain cancer treatment options; and (2) to actively engage worldwide resources to drive innovation and investment to battle brain cancer.



