The Tao of Drucker: Lessons For Drug Developers from GLP-1

David Shaywitz
The two broad categories of medical discovery that command the most attention are insights resulting from rare, informative genetic conditions (see here) and advances resulting from fortuitous observations.
A canonical example of the value of extreme genetic phenotypes is the patient with familial hypercholesterolemia who inspired Brown and Goldstein’s scientific pursuit of cholesterol metabolism and led to the statins. Similarly, Vertex’s promising pain medicine was directly inspired by rare genetic conditions associated with pain hypersensitivity and hyposensitivity.
Meanwhile, as we’ve discussed frequently in this column, many medicines, particularly in neuroscience, have been discovered by “happy accidents” – tricyclic antidepressants are one example.
Decades of Painstaking Science
But GLP-1 medicines like semaglutide (Wegovy) and tirzepatide (Zepbound) do not fall into either of these categories. Their development reflects decades of meticulous biology and physiology, of researchers working slowly and painstakingly through the complicated science.
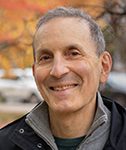
Daniel Drucker, professor of medicine, Lunenfeld Tanenbaum Research Institute of Mt. Sinai Hospital and the University of Toronto.
As pioneering researcher Daniel Drucker and colleagues wrote in a comprehensive review in 2017, “the field was built slowly with a series of non flashy yet solid studies examining the physiology, pharmacology, and pleiotropic actions of native GLP-1 and multiple GLP-1R agonists.”
Drucker notes that most papers in the GLP-1 field (at least until recently, one imagines) “were published in traditional physiology or endocrinology subspecialty journals and might be described as ‘descriptive’ or ‘incremental’ by many colleagues.”
His summary:
“Taken together, the story of discovery and characterization of the GLP’s highlights how old-fashioned biochemistry, physiology, molecular biology, and traditional analyses of hormone action provides a firm scientific foundation for the development of multiple novel therapeutics for the treatment of obesity, diabetes, and intestinal disorders.”
To put a finer point on it: genetics were not a key component of the GLP-1 story. Drucker explicitly pointed this out in his interview with Eric Topol (discussed in previous column), noting that physiologically, removal of GLP-1 or GLP-1 receptor doesn’t seem to have profound consequences. In contrast, molecules identified through genetic analysis, like leptin, have not proven to be of great therapeutic utility.
Similarly, the potential of GLP-1 medicines to cause weight loss was also not a happy accident – rather, it was seen from some of the earliest rodent studies of GLP-1, and a key thesis of the Novo GLP-1 program from the earliest days.
Key Enablers and Challenges
There were some lucky breaks, to be sure.
For one, as discussed in my last column, the adverse effects associated with GLP-1 initiation – nausea and vomiting in particular – generally wane over time, while the therapeutic effect (suppression of appetite) endures.
The biology could easily have gone the opposite way.
Also helpful: encouraging results from large cardiovascular outcome studies for long-acting GLP-1 medicines used for the treatment of diabetes (high-risk patients were found to have a significantly lower rate of adverse cardiovascular events – here, here).
These results, together with a decade of reassuring experience using GLP-1. The first, exenatide (Byetta), was approved by the FDA for use in diabetes in 2005. That molecule, originally a twice-daily injection and then formulated into a LAR version allowing once-weekly injection, helped provide confidence in the safety of this class.
Weight loss was consistently observed in patients with type 2 diabetes. The clean safety profile over time, combined with the long-term cardiovascular benefit, helped encourage companies to take a shot at a much larger patient population – people who are overweight or obese but don’t have diabetes.
Drucker acknowledges that translation of promising GLP-1 science into approved therapeutics was a particularly challenging task that required decades.
He cites several hurdles, including:
- Need for a longer-acting peptide (endogenous GLP-1 has an incredibly short half-life in the blood – only about two minutes); legendary Novo researcher Lotte Bjerre Knudsen famously spent years focused on figuring out how to create a longer-lasting therapeutic version this before finally developing a solution that become liraglutide (Victoza), a once-daily injection.
- Need to figure out dosing to address GI side effects; Drucker points out that in every clinical study, GLP-1 medicines cause GI discomfort including nausea and vomiting; eventually, Drucker says, researchers recognized that these side effects can be significantly mitigated through slow titration.
- Need for better assay reagents to detect levels of key molecules like GLP-1, GLP-2, and their receptors. Some large pharmas have analytic lab groups specifically focused on developing such tests for R&D; I recall a particularly capable team at Merck Research Labs in Rahway, NJ when I was there nearly 20 years ago.
New diabetes medicines – as well as potential obesity medicines – also require large cardiovascular outcome trials, to prove that the benefit delivered by these medicines outweigh any risk.
These concerns were motivated on the diabetes side by the experience of GSK’s rosiglitazone (Avandia), an insulin sensitizer which seemed to have a positive effect on diabetes parameters but, unexpectedly, a negative effect on cardiovascular outcomes. The high-profile safety controversy led the FDA to mandate cardiovascular outcome trials for future diabetes medicines – a move that added considerable time and cost to type 2 diabetes R&D programs.
Obesity medicines have long concerned regulators both because of the perception that they might be widely utilized as so-called lifestyle medicines, and more specifically because of the experience with the combined use of two drugs individually approved by the FDA, fenfluramine and phentermine. Used together (“fen-phen”), the combo caused some patients to develop valvular heart disease and pulmonary hypertension.
The key point here is that in many ways, GLP-1 drugs were ideally suited for large pharmas, given the time, resources, and range of expertise required to address all of these drug development challenges.
Lessons for Drug Developers
I asked Drucker what he saw as the key lessons for drug development. He cited three.
- “We should embrace multiple lines of evidence, and not just pursue human genetics-based leads”
- “Nice to use human genetics to screen out for worrisome oppositional signals or for supportive directional biology but not exclusively as a must-have criteria (or we would not have SGLT2i in heart and kidney disease, or GLP-1RAs etc)”
- “The solid reproducible non-flashy tortoise (careful papers in solid mid-tier journals) often beats the spectacular Nature/Science/Cell”
There may be an addition lesson as well.
In reviewing Drucker’s many publications, I was struck by the insight and brilliance that seemed to be required to drive the science in this complicated area. Yet when I put this to Drucker, he suggested instead that the most important attributes he’s brought to the field were his tendency to be “careful, persistent, and tenacious.”
I suspect these characteristics apply to the vast majority of successful drug developers.
We’re often attracted to the idea of science and drug development advancing through a series of brilliant ideas, eureka moments, and incandescent insights. Without question, narratives with these features make compelling stories.
Yet in the case of the GLP-1s, a category of medicine that is poised to transform everything in our world, these blockbuster medicines seem to have resulted from something quite different: decades of slow, determined science, both on the part of academics like Drucker, and companies like Novo and Lilly, patiently and deliberately nudging the work relentlessly forward.
Prediction is Hard
Finally, just to emphasize how difficult the future is to predict in medicine and science, even by the most informed experts, I feel obliged to call out a particularly revealing sentence from Drucker’s 2017 review.
Drucker writes, “market penetration for many GLP-1R agonists remains disappointing, raising questions about the potential clinical appeal, expense, and commercial success of newer formulations.”
In other words, as recently as 2017 — twelve years after the first FDA-approved GLP-1 medicine, exenatide (Byetta) for diabetes, and three years after the approval of liraglutide for obesity (marketed as Saxenda), after previous approval for diabetes (as Victoza) — it was clearly not a foregone conclusion that GLP-1 molecules were tracking to be the blockbuster obesity drugs they are today.

Michael Moritz
As legendary Sequoia VC Michael Moritz said (and as I recently discussed here), even great successes aren’t obvious early on: “I have never been involved in an investment that became a very successful business without fearing earlier that the business was going to fail, not even once.”
The problem, as Judah Folkman observed, is that to succeed, you have to proceed with conviction, but you don’t know until the end (in the case of the GLP-1 drugs, the randomized controlled trials demonstrating profound weight loss) whether you’re persistent or obstinate.
So where does this leave R&D leaders?
One thought: we should be humbled by the challenges of forecasting, cognizant of the limitations of genetics (useful as it often can be) or of any single approach to drug discovery, inspired by accomplishments of determined academic researchers and pharmaceutical scientists, awed by the intriguing complexity of human biology, and deeply grateful for our collective opportunity, as contemporary drug developers with an unprecedented set of tools and capabilities, to fashion transformative new medicines for patients.





