The Data Are Telling Us to Prepare for a Difficult Fall
PEARLS BEFORE SWINE © 2020 Stephan Pastis. Reprinted by permission of ANDREWS MCMEEL SYNDICATION. All rights reserved.

Otello Stampacchia, founder, Omega Funds (illustration by Praveen Tipirneni)
I could not resist using the above, peerless comic strip from Stephan Pastis. Indeed, the two “plagues” are not just co-existing, but they are mutually reinforcing each other and making things worse.
We should take the “great wise ass on the hill” seriously and invest in science and (investigative, high quality) journalism.
About two months ago, I wrote here about “How We Are Losing the Fight Against the Virus.” At that time, the US had 2.5 million confirmed cases of COVID-19 and reported 126,000 deaths. As of this writing, we now have tallied up more than 6 million confirmed cases, and 183,000 deaths.
Sadly, those numbers will continue to grow this fall, based on my latest look at the relevant work in epidemiology, virology and immunology (and the social-political vibes you get from watching too much cable news).
I am dividing today’s contribution in four parts:
- Where things stand (focusing mostly on the US)
- What have we learned since the beginning of the pandemic
- What we still do not know
- Some thoughts and forecasts for the fall season
If you are, like most people reading Timmerman Report, up to date with the zeitgeist, I suggest perhaps you skip parts 1) and 2) (though a refresher never hurts) and jump to part 3).
Where things stand
![]()
The above picture is from the COVID Tracking Project (@COVID19Tracking): after a worrying summer that saw 7-days rolling averages of confirmed cases exceed 60,000/day for several weeks, and rolling averages of deaths exceed 1,000/ day, the situation appears to be stabilizing / mildly improving, though on a much higher plateau than in May. Rolling averages for hospitalizations and percentage of positive tests are also showing improvements, though, again, at levels that are far from reassuring (roughly around 40,000 positive cases / day and ~900 deaths / day).
Now that summer is winding down and schools, universities and workplaces are moving back into the rhythms of fall, people want to know what to expect.
It’s going to be painful.
I’ve been following an open-source AI-driven model from Youyang Gu which has been relatively accurate to date and is followed by the well-known statistical modeler Nate Silver at FiveThirtyEight.
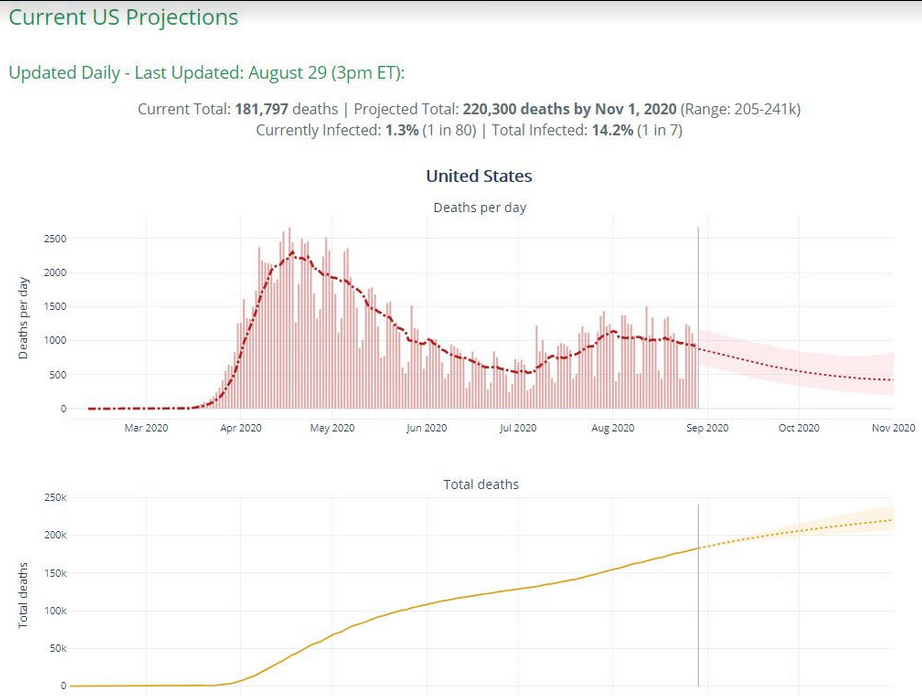
Sadly, the model forecasts roughly 220,000 deaths by November 1st, from a current (already very grim) body count of over 180,000 confirmed cases. Please note that the current confirmed toll is already DOUBLE the number of US servicemen who died in Vietnam, Afghanistan and Iraq combined, and with no signs of stopping. (The US death toll for World War II was about 400,000).
Add to this the (very roughly) 50,000 excess deaths that are very likely already attributable to COVID-19, and the toll is very heavy indeed. This is not “normal”, it is not even remotely close to (non-pandemic) seasonal flu, and we must resist the (all too human) tendency to become numb and fatalistic about this sorry state of affairs.
According to the same model, the current best estimate of cumulative American COVID-19 infections is (roughly) 14% (close to 47 million out of 330 million people). We are (obviously, but it needs to be stated clearly) nowhere near the >70% of the population needed to achieve “herd immunity”. Please remember also that the death toll does not take into account the (unclear, but significant) number of #LongCovid sufferers (patients who have recovered from the infection but suffer long term, serious health consequences). Even ignoring all that resulting chronic disease with COVID “long haulers,” and using some very, very rough math, “letting it rip” (letting the pandemic propagate without any attempt at mitigating its spread) can lead to ~800,000-900,000 total confirmed US fatalities (more if some hospital systems become overwhelmed; possibly *many* more if we try to input “excess deaths” in the calculation).
To put this into a broader context: in the 5 days prior to Sunday, Aug. 30, the largest European countries (with a population total of 340M, roughly equivalent to the US’ 330M), reported a combined 250 deaths. During that same period, the US reported 5,500+ deaths. When you look at the death toll, the pandemic at this point is about 20x worse in the US.
This is staggering, and will have implications for the upcoming autumn.
What have we learned since the beginning of the pandemic
I will attempt to summarize some of the knowledge / facts accumulated on the virus and its properties / means of propagation (and implications thereof) since the beginning of the pandemic.
a) Deaths lag hospitalizations; hospitalizations lag confirmed cases increases: the steep increase in number of cases in the US observed in the early summer led, predictably, after several weeks, to an increase in hospitalizations and then in subsequent deaths. There is an obvious lag between these events, caused by several factors: i) as the infection spreads first in the younger, less vulnerable (but not *invulnerable*) strata of the population; ii) as (unconscionable) delays in test results do not give us an accurate and timely picture of the infections spreading, and, finally (and even more unconscionably) iii) as it might take several *weeks* to report COVID-related deaths (a particular dishonorable mention to the Sunshine State, Florida, for the egregious delays, if not outright obstructionism, in reporting deaths). Remember that we are all actually living in the future versus what we normally perceive to be the present (meaning, what we could perceive the current status of the pandemic spread to be: human beings are particularly prone to recency biases). It is of particular concern when, in areas where tests are performed at scale and some speed, positive rates increase quickly. In such situations, measures such as localized / temporary lock-downs / further enforcing of social distancing / obligatory mask wearing in public are likely warranted (the latter should be enforced nation-wide ASAP).
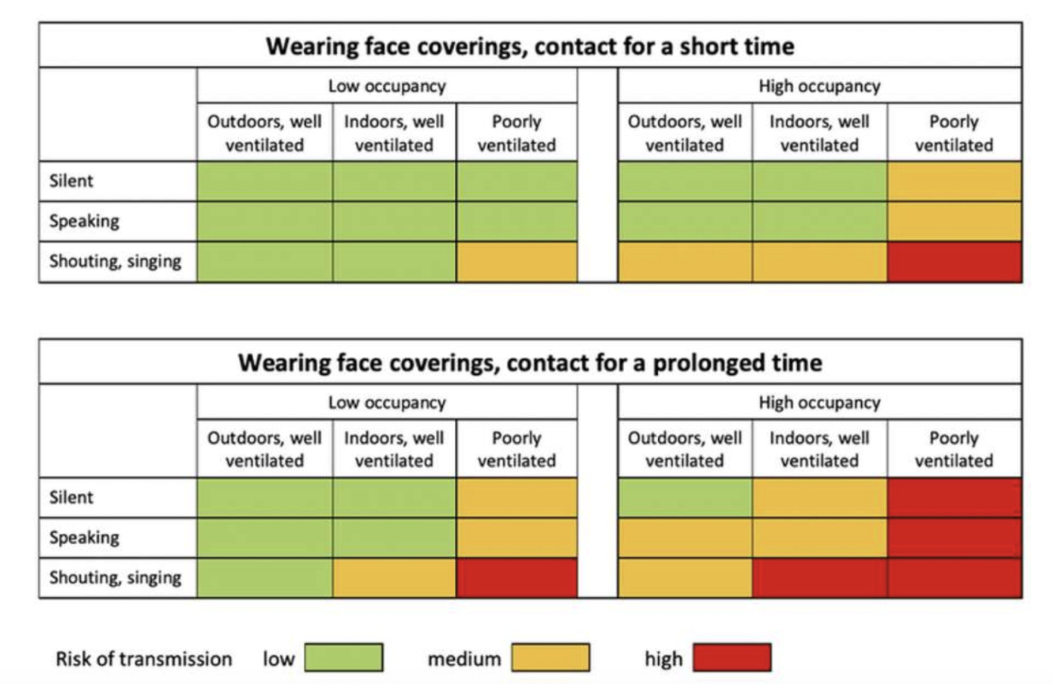
b) This is a very infective virus: It is not as bad as measles, but it is very transmissible, especially in indoor, crowded, poorly ventilated environments. You have heard (am sure) about the dreaded R0 (R “naught”) number. Crucially, R0 is not a fixed number, but it is influenced by many factors, including human behavior (masks…) and context in which a potential transmission could occur (shouting / singing in an small / contained indoor space). The virus is spread by droplets / aerosol particles generated by breathing / talking loudly from an infected person. Worryingly enough, there is now emerging evidence that such droplets can also propagate the infection by connecting with unprotected ocular surfaces (your eyes).
By now, you should also be familiar with the importance of “super-spreading events” in transmitting / propagating the virus. As little as 10% of infected individuals could be the source of ~80% of overall infections, again especially in specific environments / context (indoor, poorly ventilated, talking loudly / singing, no masks): for example, a wedding in rural Maine, an area as yet untouched by the pandemic, led to a large outbreak in the state.
Another extremely well-researched example, very close to home for me and for many readers of Timmerman Report, was the meeting of Biogen’s executive management in Boston towards the end of February (the meeting ended on Feb 27th): the event was attended by ~175 people, from different regions in the US as well as from other countries (including Italy). Scientists have estimated that over 20,000 individual infections were originated from that single conference and then spread all across the globe.
Which leads us to:
c) Non-Pharmaceutical Interventions (NPIs) are very effective in preventing viral spread: social distancing and, especially, wearing masks / face shields in indoor areas have been proven (by a whole body of scientific literature, on this pandemic and others before it) as being very effective in preventing transmission. The graph below is a great summary of the transmission risk in various circumstances and could act as a very rough guideline (always wear a mask anyway). Please note that everything is relative and highly context-dependent: if you are in an area of high prevalence of infections (Miami-Dade County in Florida, for example, or NYC during the peak of the pandemic there in March), even low-risk endeavors, if repeated many times and by a highly susceptible individual can lead to infection. Remember the probabilities here are additive. I am not going to go into which type of masks are most effective but they are an essential component. In addition, face masks also help in reducing the amount of virus that you are infected by (viral inoculum, sometimes confused with viral load), which leads to this one essential point below:
d) Viral inoculum size is very important (and may be the factor making the difference between you ending up in the hospital or just walking it off): forgive me for perhaps stating the obvious here, but I feel this topic, of paramount importance, has not been discussed much (if at all) in the general discourse surrounding the pandemic. People seem to only assume binary outcomes from encountering the virus: you either get infected or not, and then, if you get infected, you either die or survive. This is *OBVIOUSLY* not the case (not sure if you can picture me rolling my eyes right now, but, I assure you, it is happening). How much virus you are exposed to at the beginning of your infection (viral “inoculum”) has a strong correlation with the subsequent severity of your symptoms. We have known this for a while, and yet, we are still having these inane / insane and sometime unhinged discussions / fights (including at various stores across the country) about how the obligations to wear masks infringe on people’s civic liberties. Masks do, at the very least, SUBSTANTIALLY reduce the viral inoculum you are exposed to in an infective situation, and therefore *will* either i) prevent the (non-infectious) wearer from catching a potentially lethal dose of the virus or ii) prevent the (infectious) wearer from spreading a potentially lethal dose of the virus in his/her surroundings. I honestly cannot believe we are still debating this stuff 6 months into a pandemic, but there you have it.
e) The virus is not becoming less lethal over time / the virus has not mutated into a (measurably) milder version: the (very much welcome) reduction in the mortality rates that you are seeing across countries (most of them developed: emerging countries are still seeing very high case fatality rates: see Mexico, Peru, India) is because of a variety of cumulative factors: hospitals / caregivers are no longer overwhelmed; a larger percentage of the population now being infected is younger / with less co-morbidities and risk factors; practitioners have learned / shared more information on how to deal with severely ill patients (for example, by not putting them on ventilators immediately; for those of you with an interest, I suggest joining the slack channels used to exchange know-how and tips by healthcare practitioners); more people are wearing masks / being more careful in their behaviors and therefore are being exposed to lower viral inocula when infected; finally, a few pharmaceutical interventions have since become available and are making an impact (especially dexamethasone), and with more to come: People have been focusing a lot (for good reason) on vaccines, but there is a whole bunch of other stuff that might show its effectiveness before they become widely available. As any rational person would (should?) tell you, in a(ny) pandemic you do not want to get sick early. If you’re going to get sick, it’s better that it happen later, when healthcare professionals know more about the virus and its effects.
f) There is no pre-existing, foolproof, 100% protective “immunity” to this virus. I have seen over the last few weeks the spreading of this fascinating, completely unproven “theory” that there is a large amount of existing immunity to COVID-19 in the population due to the fact that, supposedly, up to 50% of people have T cells with cross-reactivity (in Petri dishes, in a lab) to this virus because of previous exposure to other (seasonal) coronaviruses. This reminds me of the late ‘90s, when curing cancer in mice was enough to make stock prices for certain (mildly overpromoting) biotech companies skyrocket… (yes, I know this statement ages me quite a bit, thanks very much). Even given this (completely unproven) “theory” (I think “opinion” might be closer to the mark) the benefit of the doubt, again we come back to the *fact* that a smaller viral inoculum (and subsequent viral load in your bloodstream) is probably more important in determining your progression towards the worst symptoms. Even some mild degree of cross-reactivity and therefore (possibly, not surely) protection will not help you if you are inhaling infectious particles by the millions without masks at an (indoor, poorly ventilated) bar. In the words of Ricky Gervais (if you do not watch his comedy stand-ups, you should): “You can have your own opinions, but you cannot have your own facts”.
g) Children (especially very young children) are not, by and large, severely affected by the virus: what I mean by saying “by and large”, is that they are not as affected as adults, probability-wise. There is, also in children, a continuum in the risk probability, again increasing with age, and with other pre-conditions predisposing to severe symptoms (obesity etc.). That said, the risk is not exactly zero even for very young children. To provide some quantification of the probabilities here, Dr. Stephanie Graff (@DrSGraff), described a recent State of Florida pediatric report (using data since March)… OK, HOLD ON. I know what you are thinking. So let me address the elephant in the room here first: far be it from me to rely upon, let alone celebrate, “Florida statistics” on the pandemic, which is as close to an oxymoron as I can think of, but this is all I got so far. At any rate, according to said (possibly very flawed) Florida statistics, 48,928 children statewide have tested positive; of these, 600 have been hospitalized (~1.2%), with most of them recovering, and 8 have tragically died (~0.01%). 50 children <18 have been diagnosed with MIS-C, which is a severe inflammatory disorder caused by the virus (~0.1%, or 1/1000 for those of you who suck at math). I have not been blessed with children, so will leave to parents their own risk-reward calculations analysis. At any rate, it is also abundantly clear that children are infected by the virus and can transmit it, sometimes very efficiently: young, college-age adults effectively seem to transmit as well as older adults. This has severe implications for community transmission as soon as schools reopen (see below), and particularly for inter-generational households with grandparents or people with other pre-existing conditions.
What we still do not know
Most of the unknowns that still plague us are related to this incredibly complex organ of the human body, the immune system. This is a new virus for the human species, and, notwithstanding the incredible progress made to date, there are still lots of things we do not know, some of which are (unfortunately) essential before being able to plan a return to some semblance of normal life.
a) How long does immunity last? In early July, a British study pre-print showed declines in neutralizing antibody titers (antibody amounts / volume of blood) observed during a ~3 months follow up period post-infection. Cue (predictably) apocalyptic commentaries. However, there are reasons (I know, this is unlike me, but bear with it for a bit) to be a bit less pessimistic: as eloquently described by Derek Thompson in The Atlantic in this very thoughtful piece as well as by his (very witty) colleague Ed Yong in many great articles (this one in particular is worth a read) the immune system is extremely complex and has many components. First, even a lower antibody titer later on might still be sufficient to forestall a severe re-infection (see below) DEPENDING ON THE VIRAL INOCULUM (see? Keep wearing a mask please). Also, the authors of the British study only looked at B cell antibody responses, and did not measure T cell responses (to be fair, that is a much harder measurement to make): there are reasons to believe that T cell responses might provide the strongest / longest-lasting immunity to COVID-19 (read here if you want to geek out). Perhaps some very rough calculations might also provide some guidance: we know that existing, seasonal coronaviruses (responsible for ~25% of seasonal common colds) are capable of re-infecting people every year or so which means immunity might last for a few months; on the other hand, SARS and MERS (the other recent coronavirus epidemics) *seem* to provide some degree of immunity for ~24 months. That said, both SARS and MERS only infected (luckily: their fatality rate was very high) a few individuals, so we do not have a deep data set to use here. If I were a betting man, I would work under the operating assumption that exposure to infection (and subsequent recovery) might confer some protection for anywhere between 12 and 24 months. The uncertainty is due to myriad factors (how much virus were you exposed to; the infected individual’s sex and the overall state of his / her immune system; the amount of virus exposed to in a subsequent re-infection; etc.). Which brings us to the latest developments:
b) People can get re-infected: note, this should technically be in section 2), but it is a very new development and there is still a lot of uncertainty / debate on the possible consequences. As described by more and more reports in the last few days, there have been (some more, other less “properly” confirmed) cases of COVID-19 re-infection (in Hong Kong, Belgium, Netherlands, and now Nevada): in these cases, the virus genetic sequence in the second infection was sufficiently different from the one from the earlier infection to rule out artifacts of detection and other explanations. Before I go on, I would like to highlight the sheer “amazingness” of this: we are testing and sequencing viruses of many infected individuals, globally. This is leading us to important learnings on the virus (the above is a not-so-snide retort to people / organizations who would like to reduce testing volumes or only test symptomatic people; apparently one such organization included, until recently, the US CDC). I’d start with the (important) premise that such cases, at the population level, are in my opinion quite rare and likely to remain so and be restricted to individuals who have decided to have the questionable bad luck of i) living in areas of very high pandemic prevalence, ii) being particularly susceptible to infection, and / or iii) engage in very risky behaviors. That said, the Nevada case is of particularly concern, since the individual had much more serious / severe disease symptoms the second time around than during the first infection: normally, even if the immune response generated after the first infection is unable to prevent a second one, it should, however, conceivably, at least forestall more severe symptoms. However, as brilliantly put by Dr. Sarah Cobey (epidemiologist / evolutionary biologist from U. Chicago, quoted in the article above), “Infection is not some binary event”, and with a reinfection, “… the question is how much is the immune system getting engaged?” Which, again, takes us back to viral inoculum size and its interaction with any individual’s immune system. As a corollary of this (extremely important) topic and the consequences on testing, I would strongly suggest you follow Prof. Michael Mina on Twitter (@michaelmina_lab): in particular, this thread (on the consequences of using PCR testing alone in guiding public health decisions) is very important.
c) Implications for vaccines: the above questions have huge implications for vaccines’ development / testing / distribution logistics: if immunity generated by the virus is indeed short-lived, then we might have to become accustomed to annual booster shots, for example. Add to this huge uncertainty some other important complexities, such as i) the mRNA vaccines currently under development are likely to require -70 Celsius or -20 Celsius cold chains; ii) that as much as 30% of the US population does not believe in vaccines and, finally, and perhaps very importantly, iii) that the recent public communication blunders by the FDA and the CDC are very likely to further increase the suspicion that any vaccines approved in a hurry just ahead of a close, contested election might be more motivated by politics than science, and you have all the ingredients for a very messy situation in which not enough people get vaccinated. [Clarification: 9:34 am ET, Sept. 1. The cold chain conditions can vary depending on the mRNA vaccine candidate. A previous version of this article grouped them together.]
Some thoughts and forecasts for the fall
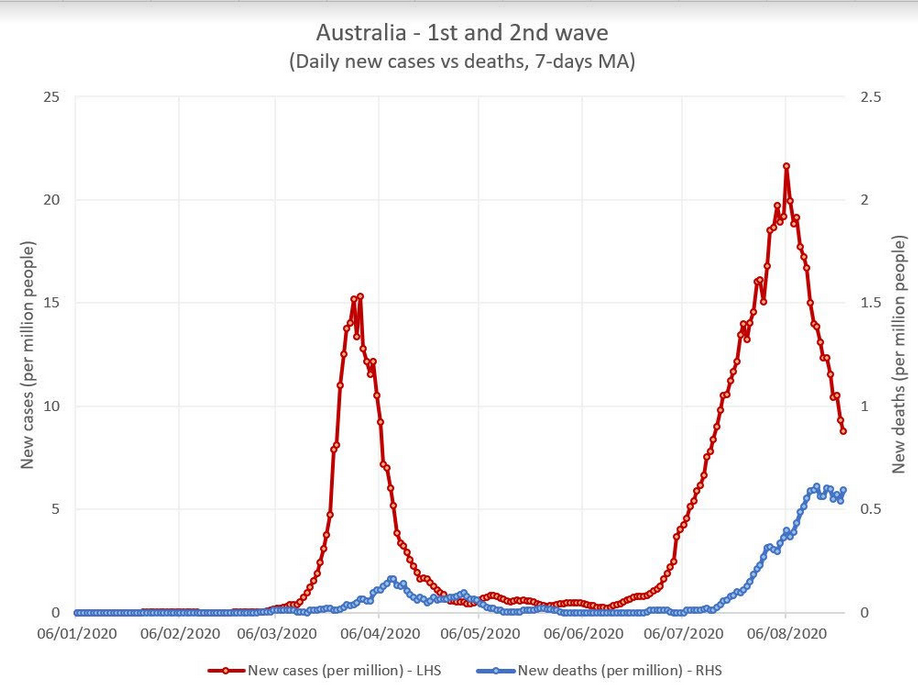
First of all, thanks for sticking with me so far. Obviously what follows is speculation. That said, I am quite concerned about the upcoming autumn / winter season. As mentioned above, the virus spreads readily and easily indoor, virus inoculum sizes become probably much bigger, and as we transition to indoor classes / living in general, in a much more generally dry environment, this is very dangerous, especially as the baseline of people already infected in the US is extremely high, driving a steady rate of community transmission (compared to most other countries). As a data point that further corroborates this, we should look at Australia: as well discussed by Silvia Merler (@SMerler), and as shown below, Australia is now truly undergoing a “second wave”, with much higher mortality rates than the first. For those of you who have not been to Australia (and who are not familiar with the fact that our planet has opposite seasons in the two hemispheres: yes, am talking to you, flat-earthers…), Australia underwent its first wave around the end of their summer and is now undergoing their second wave in their winter. With the usual lag, the second wave appears to be having a disproportionately high fatality rate vs the first. At the same time, we cannot say Australia is governed by a “negationist” government or was not warned about the virus ahead of its second wave.
To conclude, some suggestions:
a) I am extremely glad that a number of jurisdictions, including some universities, seem to be starting to administer the current season’s flu vaccine early, to prevent a flooding / overrun of their healthcare systems. I suggest this should become mandatory across the country, as soon as possible.
b) I understand the economic imperative for universities and schools to reopen (also, which parent would want their teenage children brooding at home for another year???). However, we need to be extremely mindful for the potential to further increase spread due to disorderly behavior usually associated with young adults (who are not usually showing the most compliant and obedient behavior at the best of times). It is truly amazing to observe the wave of innovative solutions being tested by various universities / colleges. Some examples of such innovation are shown here: I believe more colleges should follow the University of Arizona and University of North Carolina approach and implement wastewater virus testing from college dorms to have an early warning signal which allows them to implement contact tracing and isolation of infected / asymptomatic individuals very early in the process. Amongst many reasons to use this testing is that i) there is evidence that the virus shows in stools before or at least concomitantly with the early infectiousness period and ii) the method does not require asking teenagers to be compliant with various testing / masking / social distancing guidelines.
c) The recent launch of a fast, cheap and easy to perform antigen test format (from Abbott Laboratories) could also finally introduce a much-needed game changer on the playing field: again as discussed by Michael Mina this test format could really be useful to break transmission chains, therefore limiting / containing local outbreaks early on in their spread (which is not the case, still, with the current test types available in the US, due to their lack of reliability and the incredible, mind-boggling delays in obtaining results). This test, and hopefully soon others like it, should be deployed at scale across the country ASAP. What do I mean by “at scale”? Looking at the scope of the pandemic in the US, we should test tens of millions of people A WEEK to have a chance of contain local outbreaks / superspreading events.
d) Wear a mask.
Follow Otello Stampacchia on Twitter: @OtelloVC
This article expresses the personal views and perspectives of the author. The views and perspectives expressed here do not necessarily represent the views or perspectives of Omega Fund Management, LLC or any officer, director, partner, member, manager or employee of Omega Fund Management, LLC or any of its affiliated entities.




