Get In-depth Biotech Coverage with Timmerman Report.
22
Oct
2024
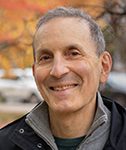
A Life in Biotech Journalism, and Reaching New Heights for Good Causes
The folks at Nucleate, the global network for young scientific entrepreneurs, asked me a bunch of interesting questions.
I was the guest on the Nucleate Podcast. This was an hourlong interview which covered some turning points in my life. I also offered some commentary on the current state of biotech.
The co-hosts wrote:
In this episode, Sam Kessel and Anastasia Janas interview Luke Timmerman, an award-winning biotech journalist and founder of the Timmerman Report, as well as host of The Long Run Podcast. They explore Luke’s non-traditional background, his curiosity, and his openness to learning, which shaped his journey to becoming a prominent figure in the biotech space. Luke shares insights into his career, discussing his book Hood, the founding of the Timmerman Report, and his podcast. He also offers his perspective on the key qualities of biotech founders and VCs, the importance of diversity, and how to unlock individuals’ full potential. Additionally, Luke discusses his passion for mountaineering and how he combined it with his work, creating the Timmerman Traverse, a series of fundraising expeditions that have raised over $12M for causes such as cancer, poverty, and sickle cell disease.
Listen to the full episode wherever you like, or at the links below.

Timmerman Report launch party, Cambridge MA. Mar. 2015