2021: The Rise of the Variants

Otello Stampacchia, founder, Omega Funds (illustration by Praveen Tipirneni)
This column will have a “glass half full / glass half empty” feeling for many readers, I fear.
Before diving deep into the troubling emergence of highly transmissible and virulent SARS-CoV-2 variants, a couple of brief reminders:
- Immunology is very complicated: for the uninitiated, please read this (always impeccably well written) piece by Ed Yong in The Atlantic.
- We still lack *a lot* of information about the virus and the immune response to it. We don’t yet know the relative role of antibody vs. T-cell responses in long-term protection against the virus. We don’t yet know whether vaccinated people are still capable of transmitting the virus to others. We know barely anything yet about the phenomenon some call “Long COVID.”
Science is moving very fast indeed, and it must continue at this relentless pace because we still have much to learn.
To drive this point home, allow me to relay a personal anecdote. I was asked to opine if it was safe for a pregnant woman (friend of a friend) to receive one of the mRNA vaccines currently being distributed in the US (she is in her third trimester). After many obvious and obligatory caveats (I am not an MD, and *definitely* not an ob/gyn, nobody should listen to me for medical prescriptions, etc etc), I mentioned that, yes, mRNA vaccines do elicit a strong immune response (the main goal with any vaccine), but that I suspect the potential risk of harm to the fetus was indeed very low (though not zero).
Two days later, WHO issued guidance “recommending generally against the use of the vaccine during pregnancy except for those at high risk of exposure or having a severe case”… Indeed, neither the ModeRNA nor the Pfizer/BioNTech mRNA vaccines have been tested so far in this population (there are plans to do so shortly). If I could print here the faceplant emoji, I would.
The WHO guidance isn’t based on any data from vaccine trials, as far as I can tell, but more out of an abundance of caution. That said, this is not straightforward, since pregnant women appear to be at higher risk of contracting severe cases of COVID-19 as well as (possibly) having a higher risk of preterm delivery (incidentally, the CDC has maintained that pregnant women should get vaccinated).
So, we still have a lot to learn. And we need to remain humble about how much we still do not (yet) know.
Some Good News
In the US, after the rise in cases and fatalities derived from Thanksgiving and Christmas mingling, we seem to be turning the corner (all the graphs below from @COVID19Tracking). It’s yet another reminder that strict Non-Pharmaceutical Interventions (NPIs) — that we knew worked 100 years ago — are still effective in preventing viral spreading via the respiratory route (see, for example, how flu transmission has basically been wiped out this season).
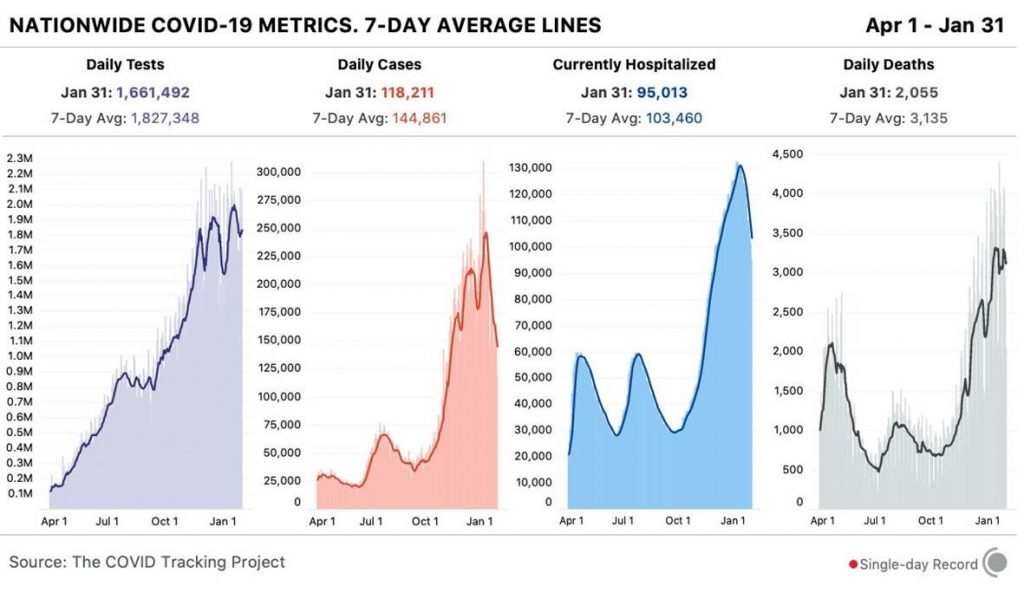
As you can see, cases / hospitalizations are coming down (though from what is an exceedingly high level): cases are definitely trending down and are ~40% below the recent peak in early-to-mid January; hospitalizations are also ~30% down from peak. Tragically, deaths remain extremely elevated at >3,000/day, and will continue to be for several (2-3) more weeks: yet another reminder that deaths are a lagging indicator resulting from infections that occurred ~4-6 weeks prior. The country will soon surpass the sober milestone of >500,000 overall fatalities.
That said, we should expect COVID-19 deaths to begin trending down soon-ish (never soon enough), assuming we continue to behave responsibly (more on this later). Encouragingly, the US administration communication policy has taken a U-turn versus the previous one (even the CDC, under new leadership, has *finally* issued a mask mandate for people using planes, trains and other public transportation).
Another, unabashedly positive piece of news: we now have positive results from two more vaccines, J&J’s and Novavax’s. This is in addition to a slew of data showing several antibodies (from Lilly and Regeneron: alone and in combination) are also extremely effective at preventing deaths and reducing hospitalizations, or in reducing overall infections within the first week, with 100% prevention of symptomatic infections.
At least one study (Regeneron’s) shows markedly decreased levels / duration of viral shedding in the asymptomatic infections that occurred in the treatment group. Of course, these antibodies need to be given at the right time, prior to hospitalization, and that’s a tricky thing for an intravenous medication (though subcutaneous formulations are in the works). But still, these are important medicines.
In case it needed to be said (again), the biotech / pharma industry is rallying at unprecedented scale and speed to provide a solution to this pandemic. What are GameStop or AMC doing in comparison??
For how I see future treatment regimens (vaccines vs antibodies vs antivirals etc), I will direct you to the “Forecasts” section of this column (at the end).
Back to the (new) vaccine data: I would like to make several (non-mutually exclusive) observations (starting with the inevitable request to compare the different vaccine results):
- As eloquently said by Kai Kupferschmidt (@kakape), as well as several other commentators, it is really not possible to compare vaccine efficacy (mRNA-based vs Novavax or J&J) with the data at our disposal (so, please: stop asking!): the mRNA vaccines were tested early on, in places lacking the variants which are circulating right now. Had they been tested in those conditions, results might look different (or perhaps much the same: we really don’t know). The headline vaccine efficacy rates that you read in the news (50% vs 80% vs 95%, say) relates to the protection conferred against infection: however, what matters *most*, as Dr. Ashish Jha (dean of Brown University’s School of Public Health) rightly said recently to the NYT: “I don’t actually care about infections. I care about hospitalizations and deaths and long-term complications.” Which brings me to:
- In the >70,000 people having received one of these 5 vaccines in controlled clinical trials, *including in geographies where the new variants are present / spreading*, as far as I can tell, there have been 0 hospitalizations / fatalities from COVID (as well as, and this bears repeating, 0 fatalities from the vaccine): basically, ALL of these vaccines work very well in preventing deaths and even severe illness (these events are measured after vaccines have had a chance to work, typically 14 days after the first shot). Even after you receive a vaccine (lucky you, BTW), you should still endeavor to behave responsibly: we do not yet know if a vaccinated person could continue spreading the infection once contracted (I know, I already said that not half a page ago, but it is worth repeating). For an example on vaccine protection, check out this thoughtful Twitter thread from Helen Branswell at STAT News on the J&J vaccine.
- In an immunologically naïve population to this virus, administration of *any* efficacious vaccine helps to increase overall population immunity. Looking at the severe manufacturing / supply chain limitations to make vaccines available to the entire world’s population, it is extremely encouraging to see the entire pharmaceutical industry joining forces to bring more manufacturing capacity online (to name but a few examples, Novartis will assist in manufacturing Pfizer/BioNTech vaccine, Bayer just announced a collaboration to increase Germany-based CureVac’s mRNA vaccine supply in 2022, etc.). I will continue to state that *everybody / everywhere should get vaccinated as soon as feasible, with whatever vaccine* available in their locale. This is also extremely important in limiting the emergence / spread of new variants (see, again, below): as Dr. Anthony Fauci just stated, “the fundamental principle of getting people vaccinated as quickly and as efficiently as you possibly can” is because it’s the “best way to prevent the further evolution of any mutation”.
Some Very Concerning News: Viral Variants Emerging
The table below (source: https://cov-lineages.org/global_report.html) shows some information about the currently-known viral variants that are spreading in different geographies: for the non-geeks/amateur virologists amongst you, B.1.1.7 is the “UK variant”, B.1.351 is the “South African variant”, and P.1 is the “Brazilian variant”.
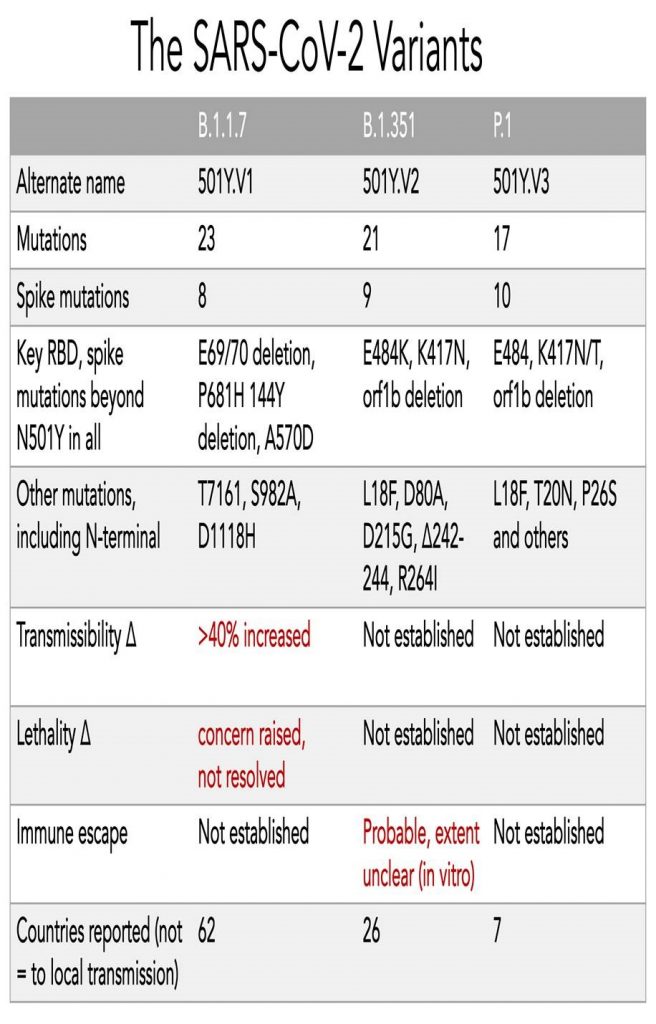
You have likely been hearing about those variants quite a bit, so will spare you a lengthy and geeky discussion. If you really want to go deep into the rabbit hole, this thread from eminent virologist Florian Krammer (@florian_krammer) does a pretty amazing job.
Here are some broader thoughts that should worry you, hopefully arranged in some sort of logical order:
- First and foremost, this pandemic is happening in unprecedented conditions. As I discussed recently with a friend from the pandemic response frontline, there is likely no precedent to this in humanity’s history: with so many individuals infected at the same time, and with widely available mass transportation / (fast) travel amongst regions / continents. As a (very rough) calculation, there have been ~100M confirmed infections to date worldwide. Knowing that there was very little diagnostic capacity (criminally so in the US) in the early phases of the pandemic, and that it is still the case in large countries / continents (there is practically 0 screening ongoing in India and the African continent, for example), it is probably safe to assume >500M people have been infected in the course of the last 10 months or so (out of a global population of ~8 billion). Worryingly, there seems to be evidence that people can be re-infected with some of the new variants (see Novavax results in South Africa and Brazil data below).
- The UK variant, for example, is very transmissible indeed (we do not yet know about the others, but I suspect they are too): starting from a “Wild Type” virus isoform that already has an R0 well in excess of 2 (vastly exceeding flu), B.1.1.7 seems to add an additional 40-60% increase in infectiousness. For a viral pandemic spreading at an exponential rate, adding a compounding 40%+ increase in transmissibility is scary. The UK variant has so far managed to colonize the landscape wherever it is present in a very short time (the curves for diffusion of that variant in Ireland and London are practically vertical). This leads to a much higher number of infected individuals in a shorter period of time, thereby leading to (many) more hospitalizations / fatalities. Hospitals simply cannot keep up with a virus that spreads this fast. The data on disease severity with this variant aren’t yet conclusive, but it appears (caveat emptor applies here) that this variant does not seem to cause more severe disease per se: so, perhaps this variant has evolved to increase the amount of viral shedding after infection.
- As of this writing, 11 cases of the South African variant have been discovered in England as well, without any direct links to its country of origin. And we are only aware of it because England is responsible for ~50% of all viral genomes sequenced to date! Not to state the obvious, but the fact that the variant was originally discovered in samples from South Africa, does not mean it *started or even stayed* in South Africa. So it’s a bit misleading or unfair to call it the “South Africa variant.” Just as the first variants of the virus arrived in the US from multiple countries, not just from China, the South African variant has likely been circulating in Africa and other countries for a while. Banning travel from Brazil, South Africa, and England like the US did on Jan 26 to limit variant transmission is helpful, but you need to assume that these variants have already been spreading quite widely in the US in the meantime. Very few countries, with the exception of the UK as stated, are properly tracking these variants with the right sequencing / surveillance efforts: which, in the case of a country as technologically advanced and wealthy in the US, is another example of failed leadership.
- Incidentally, “vaccine nationalism”, while understandable, is ultimately self-defeating and dangerous: prioritizing vaccine supplies to developed / rich countries and letting the virus continue to expand and mutate in developing countries will condemn us to endless cycles of epidemic localized flare-ups (with associated lock-downs etc) and having to continuously play catch-up by having to adjust vaccine composition and booster shots. It’s in everyone’s interest to vaccinate as much of the world as possible, as fast as possible.
- All the variants (particularly so for the South African and Brazilian variants), have a large number of mutations, several of which are shared. “Immune escape” studies have not yet been performed against the Brazilian variant: however, a number of clinical studies and preclinical experiments (too long to list here) have been performed against the South African variant. These studies strongly suggest that variant has evolved to “evade” the immune system (or, at least, a part of it): see, for example, for the Regeneron antibody cocktail, and for the recent Novavax results. The Novavax results are quite interesting (in a horror-movie kind of way): they report that >50% of UK cases resulted from the B.1.1.7 variant (did I not say it was very transmissible?). Looking at their trial results in South Africa, 90% of the cases in trial were caused by B.1.351, and vaccine efficacy in preventing infection there dropped to 49% (remember what I said above about how efficacy is measured in these trials, though). That strongly suggests: a) the virus variants are evading the immune system, and b) “prior infection with #COVID19 may not protect against subsequent infection by the South Africa escape variant”, as mentioned by the Novavax press release. Likewise, ModeRNA showed a 6.4x drop in neutralization against the South Africa variant in their publications.
- Now for the really scary stuff: as highlighted in this Lancet article, in Manaus (Brazil, in the Amazon forest), blood donor data “indicated that 76% … of the population had been infected with SARS-CoV-2 by October, 2020… The estimated SARS-CoV-2 attack rate in Manaus would be above the theoretical herd immunity threshold (67%), given a basic case reproduction number (R0) of 3.4”. However, even after this much progress toward herd immunity, there was a substantial, abrupt increase in COVID-19 related hospital admissions in Manaus during January 2021 (while, after the previous epidemic peak of late April, 2020, hospitalizations had remained stable / fairly low from May to November, despite the relaxation of COVID-19 control measures during that period). The paper is worth a full read, but I would indicate here that a) the P.1 lineage was first discovered in Manaus; b) this variant reached a high frequency (~40%) in viral genome samples from COVID-19 cases in December, 2020, but was absent in samples collected between March and November; c) the P.1 variant shares several independently acquired mutations with B.1.1.7 and B.1.325 circulating in UK and South Africa.
Forecasts
- I believe the virus is here to stay (see Pfizer CEO’s interview with Bloomberg BusinessWeek). We messed up: early on, we should have gone for *maximum* suppression of the spreading, like China did, instead of this endless whack-a-mole cycle of lock-downs / reopenings. Masks should have been (and still should be) mandatory. And I mean, N95 masks: the new variants make fabric masks almost (not entirely) useless.
- That said, currently available (for those of you lucky enough) vaccines seem to protect strongly against severe disease, even from some of the new variants. We have other tools that are also reducing disease severity in at-risk populations (antibodies and, it is to be hoped, orally-available antivirals). There, we also messed up: funding went mostly and foremost towards vaccines, neglecting antivirals, diagnostic capacity (more on this below) and increasing manufacturing of material needed for non-pharmaceutical interventions (masks etc).
- Therefore, the first order of business is to continue to massively expand manufacturing capacity and ensure everybody is vaccinated (including in developing countries) as soon as possible. One scenario I am extremely concerned by, especially in 3-4 months as we enter spring in developed countries in the Northern Hemisphere, is the one highlighted by Prof Drosten from Charite in Berlin: namely, that “once the elderly and (maybe) part of the at-risk groups have been vaccinated, there will be immense economic, social, political and perhaps also legal pressure to end the (restrictive) corona measures. And then, huge numbers of people will become infected within just a short amount of time….” Politicians and lobbyists / interest groups are not very well equipped to listen to public health advice in a pandemic, especially after one exhausting year of isolation for the elderly and at-risk groups.
- However, vaccines will perhaps, if not very likely, not be enough. We need to stop thinking of them as the silver bullet, and start thinking of them as a (necessary, invaluable) weapon in the armory. Many other weapons need to be developed and improved. If any of you has any political connections, please spread this far and wide:
- A comprehensive, clear communication policy continuously explaining that non-pharmaceutical interventions are effective (even against the new variants);
- Prepare the research / development / regulatory / manufacturing / distribution infrastructure for the potential scenario of yearly COVID vaccinations (like for flu, and perhaps even combining it with flu); and
- Very importantly: we need to stop flying blind: we need to step up genomic surveillance of viral spreading, at the community level (sewage wastewater testing, for example) as well as at the individual level (people need to be able to get fast and reliable, PCR-grade testing at airports and other potential transportation hubs).
I leave you with a mixed message: it is stunning what human ingenuity has achieved in such a short period against this pandemic. Vaccines (and other pharmaceutical interventions) are a necessary, but not sufficient component of the effort to overcome it. Public health measures, improvements in logistics / vaccine distribution, broad / fast genome surveillance, and many other measures are also necessary.
That’s because — and it pains me to say this — this pandemic really is but a dress rehearsal. Viruses and other infectious diseases are humanity’s oldest and strongest enemy.
We need to win this battle and prepare for the inevitable, bloodier wars that are surely coming.
Postscript
[Added: 9 am ET Feb. 2] Within hours after this column went to “print,” there is now evidence that the UK variant B.1.1.7 has picked up the E484K mutation (linked to some degree of ability to evade the immune system in the South African and Brazilian variants): and for a more thoughtful / full thread, please check out this from @kakape. This is pure speculation at this stage, but it feels sensible to infer that this viral mutation confers an evolutionary advantage in populations with some degree of existing immunity (UK, South Africa and Brazil were hit extremely hard in the first wave of infections in the Spring of 2020).
I will leave you (again) with this quote from Kai Kupferschmidt: “this virus is telling us again and again, that it will gladly take any opportunity we allow it of spreading and replicating to evolve and make our lives even harder.”
In retrospect, I now wish that the entire planet would have gotten into a synchronized and strictly enforced lockdown for 3 weeks or so in early March…




