Get In-depth Biotech Coverage with Timmerman Report.
11
Mar
2021
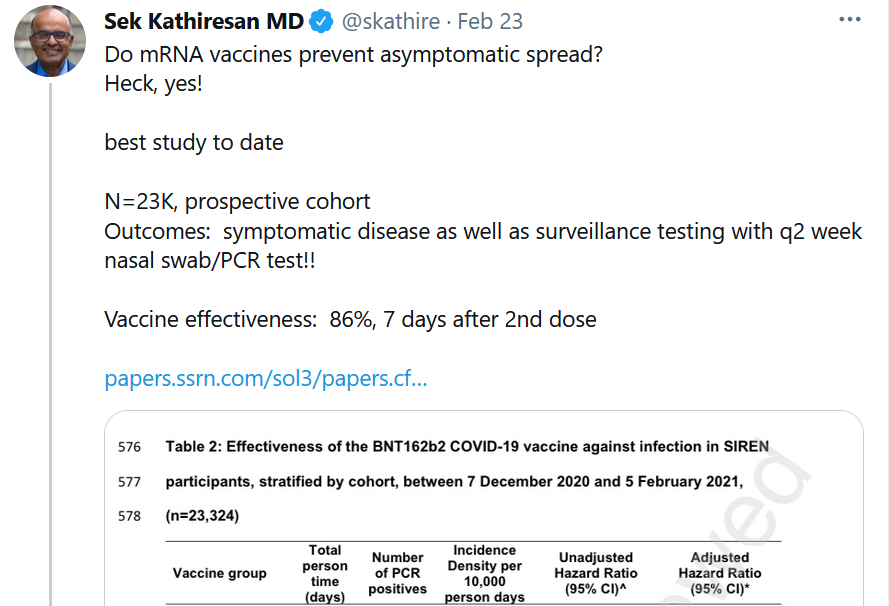
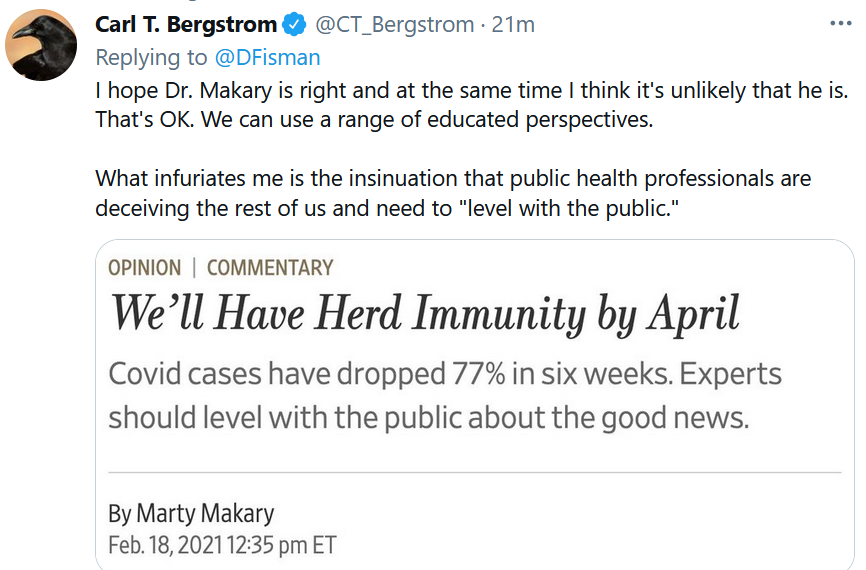
Novavax Shines, VIR Antibody Stays in the Game, and CDC Lightens Up
Please subscribe and tell your friends why it’s worthwhile. Quality journalism costs money. When you subscribe to Timmerman Report at $169 per year, you reward quality independent biotech reporting, and encourage more.