Get In-depth Biotech Coverage with Timmerman Report.
27
Nov
2024
What Should We Pay for a Good Death?
The intensive care unit in a hospital is a place where hope and despair whisper back and forth in the air.
For Richard, the emotional seesaw was becoming all too familiar. This was his third ICU stay in a month, and the ninth brush with life and death from pulmonary arterial hypertension. No matter how hard the day was, he remained determined to live happily. He’d belt out Rolling Stones songs at full volume, drowning out the hum of machines.

Dr. Lindsey Ulin, palliative care fellow, Massachusetts General Hospital and Dana Farber Cancer Institute.
I could never quite bring myself to disturb him, so I’d gently slide the door closed, not wanting to disrupt his joy.
His prognosis was grim. High-flow oxygen and a constant Remodulin infusion were his companions. Even so, when he got out of the hospital, he would quickly hop on planes and trains to see the world. His will to live a good life was powerful. So when it came time to address his recent escalation in medical care, I wasn’t surprised that Richard put up another fight.
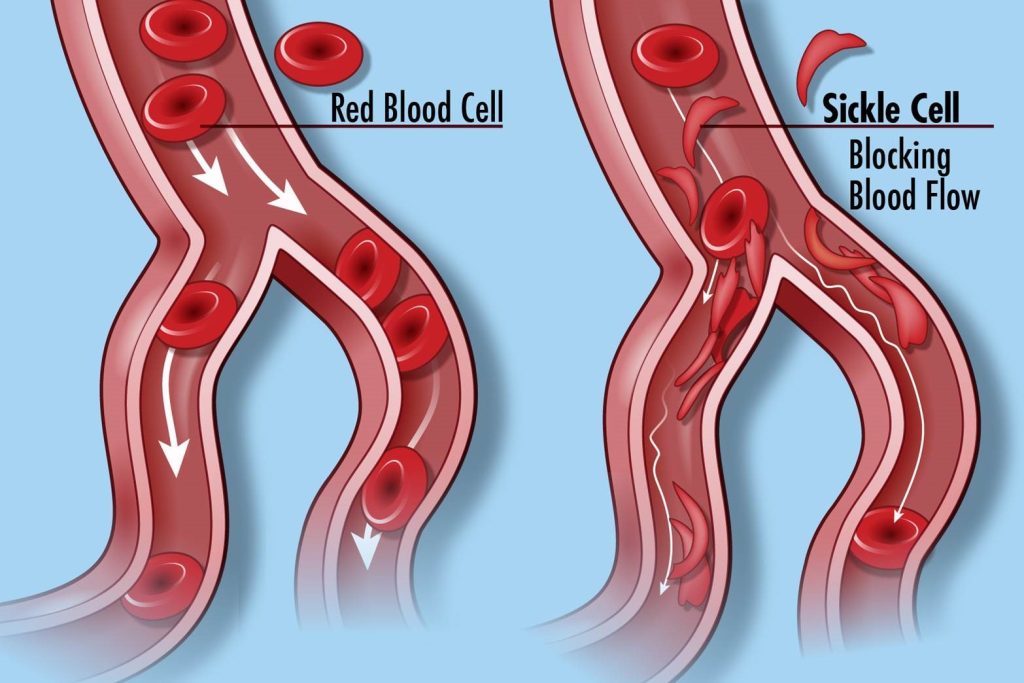
Pulmonary arterial hypertension (PAH) is a terminal illness, manageable through medications like treprostinil in the injectable or inhalable forms (Remodulin) and (Tyvaso). But these drugs only buy some time. The disease is irreversible without a lung transplant. For Richard, his age (80s) and medical history of other co-morbid conditions meant he was no longer a candidate for a transplant. Time was running out. We began discussing hospice care.

Dr. Jingyi Liu, a hospitalist and biopharma investor in New York City.
Hospice is both a philosophy of care and an insurance benefit. The focus of care changes from curative therapies to maximizing comfort and quality of life with an interdisciplinary team of clinicians, social workers, and chaplains. It’s an option for adults and children with a life expectancy of less than six months, but it requires making a difficult decision.
Receiving hospice care requires stopping medical treatments to help them live longer, which also may make them feel better.
This is where the H.R. 9803 Hospice Care Accountability, Reform, and Enforcement (CARE) Act, currently introduced to the US House of Representatives, comes into play.
Currently, under Medicare, hospice services are paid for at a per diem rate (~$200 per day for hospice-at-home) which must cover everything ranging from nursing care to medications to equipment.
This payment structure hasn’t evolved since the 1980s. Payments were based on a couple of assumptions. Cancer patients, for example, tended to decline and die fairly quickly. Second, there was a clear line between drugs that extend life (e.g. chemotherapy) and treatments that alleviate symptoms (e.g. opioids for pain and shortness of breath).
Advances in medicine have made this payment structure outdated. Medications like Remodulin can both reduce symptoms and extend life. It’s not a cure. Remodulin is one of a handful of treatments that isn’t covered by Medicare’s hospice payment structure because it extends life for a while, without offering hope for a cure. Inotropes and diuretics for heart failure, dialysis and related medications for kidney failure, supportive medications for liver failure, and blood transfusions for leukemia are a few other examples of medicines that reduce suffering at the end of life but aren’t covered by Medicare’s hospice payment plan because they also extend life for a while longer.
Provisions within the CARE Act could expand access to what’s called “concurrent care”. This would allow Medicare to pay for the usual hospice treatments, and a few of the others listed above that help people live better and maybe a while longer.
Interestingly, while most adults on Medicare, like Richard, cannot receive concurrent care, veterans receiving care through the Veterans Health Administration and children can. So there is a precedent.
For Richard, Remodulin made breathing easier, but it wouldn’t change the fact that he was likely to live six months or less. The dilemma was clear: stop the medication and enter hospice, but likely face death within hours, or stay on Remodulin, forgo hospice support, and hopefully have a few more weeks to months of life.
It’s a tough decision, one that weighs heavily on those who rely on medications that both alleviate symptoms and extend life.
Conversations about the end of life are never easy. But what makes them even harder is the unspoken truth: we’re forced to put a price on something we can never truly quantify—how much we’re willing to pay for someone to die well.
Healthcare costs soar as life comes to an end. Medicare data confirm that hospitalizations are the primary driver of these rising expenses. The cost of medicine is a smaller contributing factor.
Within these tough and nuanced discussions lurks a bigger question: How much are we willing to invest in giving people a good death? What’s considered a good death will be different for each of us, but we all share the same fears of dying in pain and discomfort.
When people want to continue living, we’re quick to pay the bills for treatments that offer a few more months, a few more breaths, a little more hope. But when people are ready to die, we decline to pay for medications, even if they help people live a bit longer and better.
A good death and the memory of it for loved ones left behind should count, too.
Richard decided that he wasn’t ready to unplug his Remodulin. I couldn’t blame him. With a favorite Rolling Stones song and a twirl of his motorized wheelchair, he checked himself out of the ICU.
Next stop? Las Vegas. The casinos. The flashing lights. And maybe, just maybe, a triple 7 on a slot machine.
For Richard, it wasn’t about the odds; it was about the joy and the fleeting happiness we all crave, even as his time was running out.
Dr. Ulin is a palliative care fellow at Massachusetts General Hospital and the Dana Farber Cancer Institute.
Dr. Liu is a hospitalist and biopharma investor in New York City.



























 I have always kept my business and political lives separate – and have had no trouble doing so. But now my political beliefs and my industry are threatened by the same plague.
I have always kept my business and political lives separate – and have had no trouble doing so. But now my political beliefs and my industry are threatened by the same plague.