Get In-depth Biotech Coverage with Timmerman Report.
3
May
2025
Our Collective Hope For AI in Health, Plus Explanatory Models and an Epic Podcast

David Shaywitz
A recent piece by Nathan Price captures our collective hope for AI in health with unusual clarity, even as there remains impassioned disagreement regarding how close these ambitions are to meaningful realization.
For context, Price is Professor and Co-Director of the Center for Human Healthspan at the Buck Institute for Research on Aging and CSO of Thorne, a company best known for its supplements, and which is now expanding into testing. He’s also the co-author, with Lee Hood, of the 2023 book, Age of Scientific Wellness.
Writing in MedCityNews, Price argues that AI represents a key enabler of “precision wellness.”
AI now makes true biological personalization possible by analyzing an individual’s unique genetic variants, microbiome composition, and blood markers to create lifestyle and nutrition recommendations that traditional one-size-fits-all approaches cannot match. Where conventional wisdom offers standardized solutions, your biology demands precision….
The complexity of the vast number of biological interactions creates a virtually impossible puzzle for individuals to track independently. This is precisely where AI excels — processing vast amounts of personalized data to identify which natural product combinations could work with your unique biological system.
AI enables personalization at scale, delivering both cost-effectiveness and depth of analysis….
The result transforms overwhelming complexity into simple, actionable recommendations tailored to your body’s specific needs, limitations, and opportunities.
These three conceptualizations of AI – its promise as a (1) critical complexity-management tool; (2) vital integrator of ever-larger datasets available through improved measurements techniques including digital/wearables; and (3) personalization machine — are manifesting as key themes across many health domains.
Besides wellness, recent examples include:
Nutrition: “Precision nutrition for cardiometabolic disease,” by Guasch-Ferre et al, in a recent issue of Nature Medicine.
Geromedicine: “From geroscience to precision geromedicine: Understanding and managing aging,” by Kroemer et al, in a recent issue of Cell.
Clinical Development in Biopharma: “AI: An essential tool for managing the burgeoning complexity of clinical development in pharmaceutical R&D,” which Pfizer’s Subha Madhavan and I published in Drug Discovery Today.
As Madhavan and I write,
Profound advances in biomedical science have created abundant opportunities for drug developers, who are now privileged with the responsibility of sifting through an ever-increasing number of therapeutic targets, treatment modalities, and measurement techniques in effort to deliver transformative medicines to patients. Digital technologies, particularly AI, represent a promising approach to managing the burgeoning complexity of clinical development.
There are remarkably similar themes articulated in each of these papers – namely that today, we tend to make consequential decisions in each of these domains based on heuristics, instinct, and our ability to process some fraction of the available data (which represents a tiny fraction of the theoretically obtainable data). The expectation is that we could make better decisions if we could responsibly access and thoughtfully analyze a far greater volume of every type of data, ideally collected longitudinally. The hope is that AI can profoundly enable this analysis and perhaps is already starting to do so.
Many tech optimists believe success in health is inevitable, and even on our doorstep. Deep Mind CEO Demis Hassabis recently told reporter Scott Pelley on 60 Minutes that the end of disease may be “within reach. Maybe within the next decade or so, I don’t see why not.”
In contrast, biopharma veterans tend to be more skeptical. This comes through in chemist and blogger Derek Lowe’s thoughtful response to the Hassabis interview. Our knowledge of biology’s interlocking systems is “completely inadequate to cure disease within ten years,” he writes. “And unfortunately, it’s going to be inadequate at the end of that ten years, too – I will put that marker down, although it doesn’t make me happy to do it.”
Lowe continues,
That’s because we don’t have enough pieces on the table to solve this puzzle. We don’t even have enough in most of these areas to know quite what kind of puzzle we’re even working on. Nowhere near. And AI/ML can be really, really good at rearranging the pieces we do have, in the limited little areas where we have some ground-truth knowledge about the real-world effects when you do that. But it will not just start filling in all those blank spots. That’s up to us humans. My most optimistic take on these technologies is that if things go really, really well they might be able to help guide us towards more productive research than we might otherwise have been doing, but we are going to have a lot of data to gather, a lot of answers to run down, and a lot of twists and turns and utter surprises to deal with along the way. We’re going to need a terrifying amount of new knowledge before we can actually turn to any AI/ML systems and ask them the kinds of big questions I mention above.
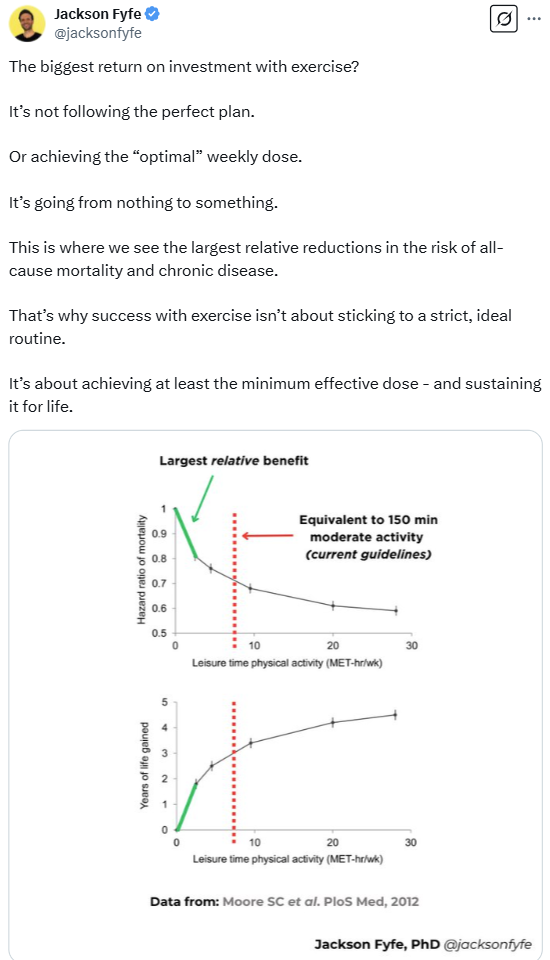
The dimension of the challenges we’re wistfully hoping AI can somehow solve is perhaps most easily appreciated in the domain of wellness, with its goal of staying healthy and preempting illness.
On the one hand, we all recognize the limitations of the familiar heuristics – eat healthily, exercise, engage with others. These can feel superficial and non-specific, the guidance not particularly customized.
Yet if you decide to make the relentless optimization of health your personal “objective function,” with every life choice adjudicated based on whether it’s likely to maximally enhance your health, you can easily lose your mind as you disappear down the rabbit hole of endless ramifications and never-ending tradeoffs.
In this context, the appeal of an algorithm that can effortlessly manage this optimization for you, personalizing and prioritizing your endless choices in an evidence-driven fashion seems enormously attractive. If only data existed to enable such assessments; at the moment, like Lowe, I’m skeptical.
Realistically, in all of the health domains we’ve discussed, the critical question isn’t so much whether we will “cure all disease” (or not), or “optimize personal wellness” (or not), but rather what are the “pockets of reducibility” (to borrow Stephen Wolfram’s term). Where will we have the requisite data – and, as Andreas Bender has discussed, a problem posed with suitable constraints — to fully leverage the power and promise of AI to move the needle in a domain of health.
Explanatory Models in Medicine, Wellness – and AI Investing
Legendary Harvard physician-anthropologist Arthur Kleinman, who delivered his Last Lecture at Harvard this past week, introduced the concept of the “explanatory model” in medicine.
As I described it a few years back, the “basic idea is that different people have different views of illness and disease, and the physician or healer needs to understand and acknowledge the patient’s model to optimize the therapeutic relationship.”
At the time, I was writing about how legendary geneticist Francis Collins was famously motivated to change his diet and exercise routine after a genetic test reportedly suggested he might be at increased risk for diabetes.
This seemed striking to me, because, as I noted,
from a medical perspective, the logic is lacking, or at least soft; most people would presumably benefit from a healthier lifestyle, whether genetic testing reveals a particular predisposition or not. Collins, a physician-scientist, shouldn’t have needed genetic testing to motivate lifestyle changes. Yet apparently, it took genetic testing because that deeply resonated with his explanatory model of illness.
The notion of explanatory models applies to our discussion of AI in health in at least two ways.
First, in the same way that Collins was motivated to adopt healthier behavior on the basis of genetic data, I can easily imagine others who might be similarly motivated because an algorithm supposedly powered by a superintelligence spits out a very specific, ostensibly precisely customized lifestyle plan.
The second application of explanatory models to AI may apply not to patients but to investors. Many tech investors are convinced that biology is poised to be disrupted by technology and technologists.
Consider these comments from noted investor (and contrarian) Peter Thiel, in the context of a 2019 interview:
Biology, I continue to think we could be doing a lot more, we could be making a lot more progress. And you know, the pessimistic version is that no, biology is just, is much harder than physics, and therefore it’s been slower going.
The more optimistic one is that the culture is just broken. We’ve had very talented people go into physics. You go into biology if you’re less talented. You can sort of think of it in Darwinian terms. You can think of biology as a selection for people with bad math genes. You know, if you’re good at math, go to math, or physics, or at least chemistry, and biology we sort of selected for all of these people who are somewhat less talented. So, that might be a cultural explanation for why it’s been been slower progress.
In other words, biology, and biomedical research has apparently been slowed by the comparatively inferior minds who’ve been attracted to it, versus the prodigies drawn to more quantitative disciplines.
The corresponding hope among many tech investors is that with the arrival of quants and their technology, including in particular AI, biomedical science can be rescued from the plodders.
Not surprisingly, many companies promoting revolutionary AI solutions to biopharma R&D have raised significant capital, especially impressive — not to mention useful — in this otherwise dour biotech market.
Recently, I saw a representative deck from one of these companies; what was striking was how the entire process of drug development had been completely reframed in a way that seemed likely to align perfectly with a tech-first view of the world.
This marketing strategy was apparently successful, since the company in question has raised considerable capital.
Yet, when I cut through all the jargon, what I saw was essentially a tried-and-true strategy – in-license, develop through value inflection, sell. Sure, maybe AI is improving this process somehow, but my suspicion is that the main function of AI in this company is serving as an attractant for a huge amount of money, which talented and seasoned drug developers (including a very experienced drug picker) can then serially deploy, with multiple shots on goal.
It’s arguably similar (as I’ve described here) to Millenium Pharmaceutical’s experience of raising lots of money through the promise of genetics and molecular profiling, and then succeeding largely on the strength of using this money to acquire LeukoSite, including (unbeknownst to them at the time of the transaction) the compound that would ultimately become the blockbuster Velcade.
In short: the idea of cleverly applying AI to pharma R&D resonates with many deep-pocketed tech investors, articulating in effect their own “explanatory model” of where the next big breakthrough may come from. Savvy biotech startups have leveraged their understanding of this investor mindset to raise significant capital and pursue what (sans AI) might be considered reasonable if fairly prosaic approaches – only now with considerable resources to put behind these efforts.
Epic Podcast
I’ve previously highlighted the Acquired podcast (what “the smartest people in the world are all listening to,” according to a 2024 Wall Street Journal “Science of Success” column by the wonderful Ben Cohen) in the context of GLP-1 and an episode they did on Novo Nordisk.
Now, the Acquired team applies their exceptional talents to unpack the story of Epic, the electronic medical records behemoth physicians love to hate (my own contributions to this dialog here, here, both co-authored with Tory Wolff of Recon Strategy). I remembered how surprised I was in 2018 when the New York Times published an adoring account of the company, and thinking, “gosh, were they taken in.”
Yet it turns out the Times may have been prescient. The Acquired episode on Epic – focusing in particular on founder and CEO Judy Faulkner as a (phenomenally successful) tech entrepreneur – was even more effusive. While the dissatisfaction among providers was noted in passing, the clear emphasis was on how brilliantly and relentlessly the company delivers for its customers.
As the hosts explicitly emphasize, Epic’s customers are manifestly not the providers whose souls (some have said) are drained by Epic, but rather by the top executives — specifically the CEO, CIO, and CFO — of academic medical centers and other healthcare companies who choose to deploy Epic.
The episode – inspiring at times, maddening at others – is nevertheless an essential listen.